Exudative AMD is managed through the application of anti-angiogenic drugs via intraocular injections directly into the vitreous cavity. The drug works by blocking the molecule responsible for the development and progression of neovascular membranes. This treatment halts exudative AMD in most cases, preserving initial vision in three out of four patients and improving it in one out of three. The effectiveness depends on how early the treatment begins and how well it is maintained to prevent irreversible damage.
To achieve these results, early diagnosis of age-related macular degeneration (AMD) is essential, even before apparent symptoms arise or in the early stages of the disease. This approach is shared by all ophthalmologists, although healthcare system limitations often prevent patients from receiving immediate treatment, allowing exudative AMD to progress and worsen. At the Institut de la Màcula, a globally recognized organization specializing in exudative AMD, we apply a differentiated treatment aimed at keeping the disease under control while preserving the highest possible level of vision for as long as possible.
Our treatment has two fundamental pillars for age-related macular degeneration (AMD):
1 – Proactive approach
To prevent relapses of exudative AMD, it is essential for the treatment to be proactive and anticipatory, ensuring that the patient receives the necessary number of intraocular injections. Unfortunately, in many countries, even in Europe, patients are undertreated and receive an average of only 6 injections over 2 years. It is estimated that 3 out of 4 patients are in this situation—or worse. According to various studies and scientific evidence, the recommended number in the first year should be at least 7 injections. At the Institut de la Màcula, we apply proactive, consensus-based protocols to optimize both the efficacy and safety of the treatment, administering the necessary number of injections for each patient with exudative AMD.
2 – Long-term treatment
The benefit obtained from treating age-related macular degeneration (AMD) must be maintained for as long as possible. Leading studies, such as those conducted by Australian research groups, show that with sufficient long-term treatment, vision can be preserved for many years. Unfortunately, this is not standard practice. At the Institut de la Màcula, we treat patients over the long term and conduct rigorous monitoring, extending the intervals between intravitreal injections for exudative AMD whenever possible, but never suspending treatment for years. This is the only way to preserve vision beyond the short term. There are no shortcuts with this disease, and attempts to observe exudative AMD without proactive treatment—trying to save on visits or injections—often lead to relapses and vision loss that cannot later be recovered.
Widespread assumptions such as “patients will lose vision within a few years no matter what” are false. At the Institut de la Màcula, we have numerous cases of patients with exudative AMD who, after more than 10 years of disease and treatment, are still able to read—one of the most complex visual tasks and one of the most valued human functions. Achieving this, however, requires great rigor and strong commitment to long-term treatment for age-related macular degeneration (AMD). Therefore, patient education and that of their support network by the retinal specialist is of crucial importance.
At the Institut de la Màcula, we know this disease well. Over the past three decades, we have actively participated in most clinical trials, described and published new findings on the pathology, contributed new treatment regimens, and advised numerous pharmaceutical companies and stakeholders in the industry on the development of new drugs.
Today, several treatments are available for exudative AMD. Lucentis (Ranibizumab) and Eylea (Aflibercept) are the two main drugs that have shown not only high efficacy over the years, but also a very high safety profile. Among other advantages, these drugs come preloaded in syringes, avoiding the need for medication handling. Bevacizumab (Avastin), a drug originally designed for intravenous use in certain cancers, is increasingly being phased out, as it is not approved for intraocular use and must be manually divided from a large vial, increasing risk.
In recent years, research has focused on developing longer-lasting drugs for the treatment of exudative AMD. A new drug, Brolucizumab (Beovu), was recently approved, but once it began to be used, severe side effects such as ocular inflammation and vasculitis appeared—effects not detected in clinical trials—making its use unjustified for the vast majority of exudative AMD patients. Another drug, Faricimab (Vabysmo), has recently been approved in several countries and will soon be available in our region. It has shown the potential for slightly longer duration in some patients and is expected to improve treatment for age-related macular degeneration (AMD).
Intravitreal injection protocol for exudative AMD:
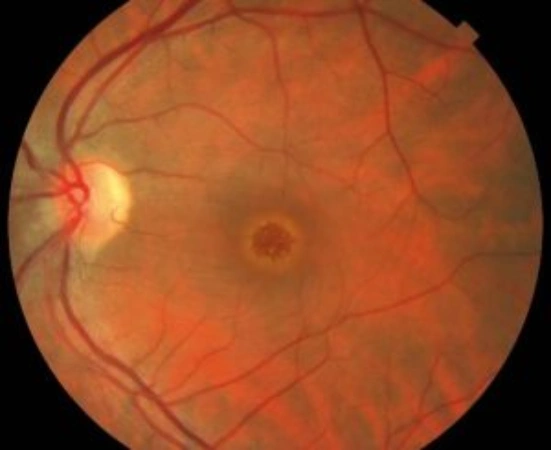
- Pre-injection evaluations: A comprehensive eye examination is essential, including fundus photography, autofluorescence imaging, optical coherence tomography (OCT), and in some cases, non-contrast OCT angiography or contrast angiography using fluorescein and indocyanine green.
- Injection procedure: The injection is performed using topical anesthesia (eye drops) and generally does not cause significant discomfort. It is a brief procedure done in-office under strict aseptic conditions.
- Precautions: Before the procedure, the eye and eyelids are thoroughly disinfected with iodine-based solutions.
- Risks: As with any procedure, the most serious risk is eye infection. However, with proper preoperative disinfection and strict adherence to aseptic protocols, the risk is extremely low—less than one case in every three thousand patients.
In some cases, patients may experience mild eye discomfort in the first few hours after the injection, typically a foreign body sensation caused by irritation from the iodine solutions used for disinfection. These symptoms usually resolve within a few hours with the application of eye drops.