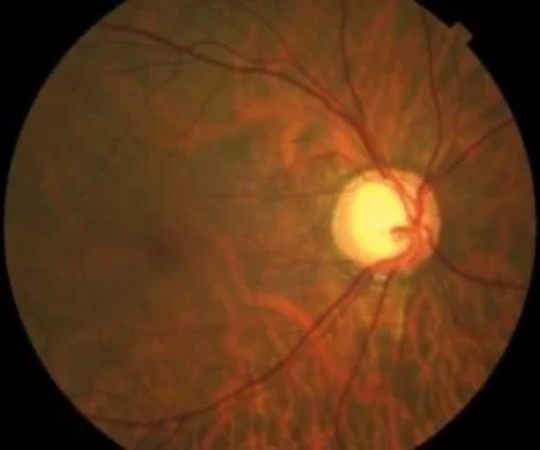
Open-angle glaucoma is an eye disease generally characterized by a pathological increase in intraocular pressure due to poor drainage of the aqueous humor, although this is not the only cause. It is an optic neuropathy marked by the progressive loss of nerve fibers and changes in the appearance of the optic nerve. If open-angle glaucoma is not treated, it can cause irreversible vision loss and even lead to blindness. It has a prevalence of 2% among patients over the age of 40 and is currently the second leading cause of blindness worldwide.
Main Risk Factors
There are several conditions associated with a higher risk of developing open-angle glaucoma:
- Ocular hypertension: intraocular pressure higher than 21 mmHg.
- Age: the risk increases from the age of 60.
- Family history: nearly quadruples the risk compared to the general population.
- High myopia.
- Thin corneal thickness.
- Vascular factors: diabetes, high blood pressure, migraines, rheumatologic diseases, among others.
- Patients taking corticosteroids.
- Signs of angle blockage in the eye: pseudoexfoliation (protein material) and pigment.
OPEN-ANGLE GLAUCOMA
The trabecular meshwork is a structure located at the iridocorneal angle responsible for draining the aqueous humor. In open-angle glaucoma, this meshwork is visible during gonioscopic examination, but it does not function properly. As a result, aqueous humor is produced faster than it is drained, accumulating in the eye and increasing pressure.
Primary open-angle glaucoma refers to cases where no direct cause of this dysfunction is identified. On the other hand, secondary open-angle glaucomas may occur when there is a clearly identifiable direct cause:
- Pseudoexfoliative glaucoma: flaky material that forms on the outer layers of the lens accumulates in the trabecular meshwork, partially blocking it and impairing drainage.
- Pigmentary glaucoma: pigment released from the iris accumulates in the trabecular meshwork, also impairing drainage.
- Neovascular glaucoma: new blood vessels form on the iris or in the eye’s drainage channels, often associated with diabetic retinopathy, central retinal vein occlusion, and ocular ischemic syndrome.
- Traumatic glaucoma: may appear immediately or years later due to angle recession.
- Corticosteroid-induced glaucoma: corticosteroids are anti-inflammatory drugs that can increase intraocular pressure.
- Uveitic glaucoma: uveitis is an inflammation of the eye that can cause high pressure either due to the inflammation itself or the treatment (corticosteroids).
This group also includes normal-tension glaucoma, which occurs in individuals with intraocular pressure equal to or below 21 mmHg who develop open-angle glaucoma with similar characteristics and symptoms to primary open-angle glaucoma. The causes are unknown, although treatments aimed at reducing eye pressure are effective in managing the condition.