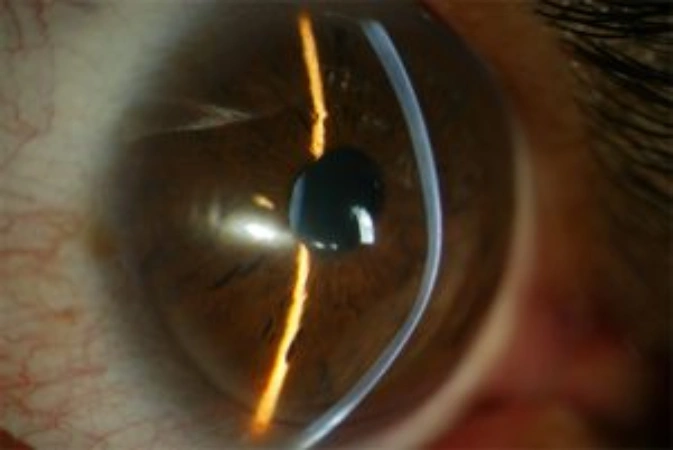
Keratoconus is the most common non-inflammatory axial corneal ectasia. It is characterized by central or inferior paracentral thinning, which causes a progressive increase in corneal curvature. This results in myopia, irregular astigmatism, and conical apical protrusion.
Keratoconus is the leading cause of corneal transplantation in young patients. The etiology is not fully known and is likely multifactorial. A positive family history has been described in 6%–8% of cases. It is likely that if corneal topography were performed on relatives of affected patients, the incidence would be higher. In other cases, it appears sporadically, linked to complex inheritance patterns that are still under investigation.
There are also cases related to ocular allergy or continuous eye rubbing. The typical form of presentation occurs at puberty and progresses over the following ten to twenty years. The rate of progression tends to be higher the younger the patient is.